How Public Health Labs Use LIS to Respond to Outbreaks
Introduction: When Time Defines Outcomes
In public health, every second counts. Whether it’s COVID-19, influenza, or an emerging pathogen, the speed and accuracy of diagnostic response determine how fast communities can contain an outbreak.
Behind every rapid test result and epidemiological report is an often unseen hero: the Laboratory Information System (LIS).
Public health labs across the country depend on LIS technology to track specimens, share data, monitor trends, and report results in real time all while maintaining compliance and data security.
This blog explores how LIS systems like Prolis empower public health labs to operate at the front lines of outbreak response turning data into action.
The Role of Public Health Laboratories in Disease Response
Public health labs are the backbone of national surveillance networks. Their responsibilities include:
- Detecting emerging infections
- Tracking disease spread across populations
- Supporting hospitals and diagnostic labs
- Coordinating with CDC and state health departments
- Ensuring data accuracy for public safety decisions
But when case volumes surge and testing demands spike, manual data entry, paper requisitions, and siloed systems can cripple response times.
That’s where an LIS transforms the landscape enabling labs to process thousands of results per day while maintaining accuracy and compliance.
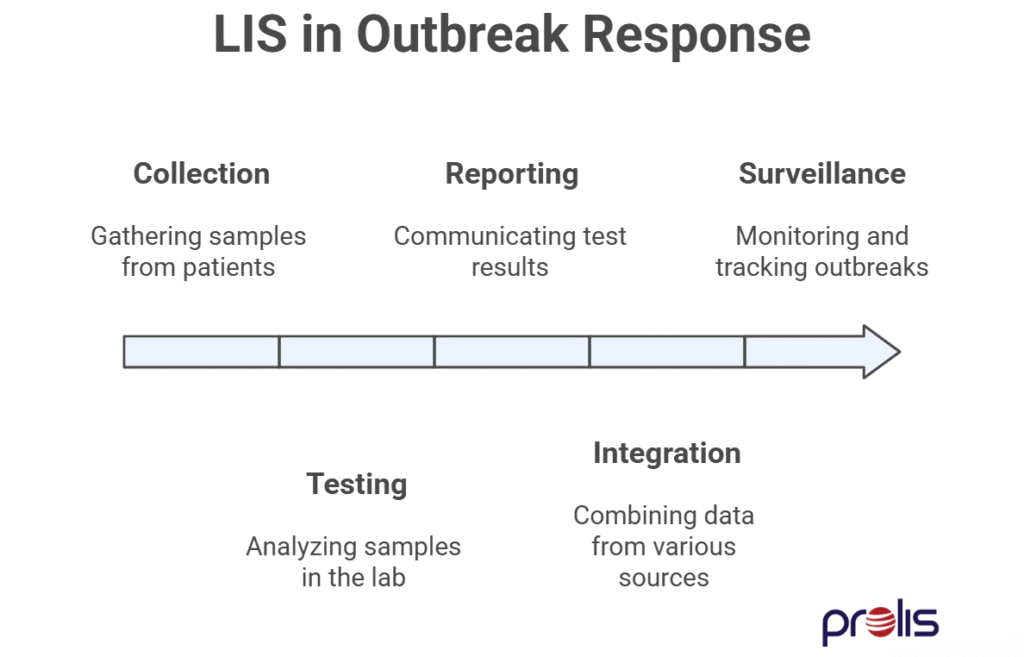
How an LIS Enhances Outbreak Response
Let’s break down the specific ways LIS technology empowers public health labs to act faster and smarter in crisis scenarios.
1. Rapid Specimen Accessioning and Tracking
During an outbreak, specimen volume multiplies overnight. An LIS automates the intake process:
- Barcode generation at collection
- Real-time accessioning with metadata (location, date, test type)
- Chain-of-custody tracking through every stage
- Flags for urgent or high-priority samples
This not only reduces labeling errors but also provides a complete trace of every specimen’s journey from patient to public health record.
2. Automated Result Management and Reporting
Manual data entry can delay reporting by hours or days unacceptable during an outbreak. An LIS automates:
- Result upload directly from analyzers
- Autoverification based on rule sets
- Report generation and routing
- Real-time notification to state or federal databases
Impact: Faster response, fewer errors, and consistent result communication to healthcare providers and agencies.
3. Integration with Surveillance and Public Health Systems
An effective LIS doesn’t work in isolation it connects with broader disease surveillance systems like:
- CDC’s National Electronic Disease Surveillance System (NEDSS)
- Health Level 7 (HL7) and FHIR data exchange standards
- State-specific disease reporting systems
These integrations enable seamless data flow between labs, hospitals, and agencies, ensuring a coordinated response.
4. Real-Time Epidemiological Dashboards
Outbreak response requires situational awareness. Modern LIS platforms like Prolis provide:
- Dashboards visualizing test positivity trends
- Geographic heat maps of case distribution
- Alerts for abnormal result patterns
- Data export tools for epidemiological modeling
These tools turn raw test data into actionable intelligence for public health decision-makers.
5. Quality Control and Biosafety Monitoring
Under pressure, labs can’t afford mistakes. LIS systems help maintain quality through:
- QC tracking and Levey-Jennings charts
- Automated calibration and maintenance logs
- Incident logging and corrective action workflows
- Role-based access control for biosecurity
This ensures that data remains reliable even when workloads surge.
6. Scalability During Surges
Outbreaks demand rapid scalability. A flexible LIS supports:
- Multi-site operations
- Cross-lab data sharing
- Rapid onboarding of new test codes
- Cloud-based access for distributed teams
Prolis, for instance, can be configured to connect multiple collection points, allowing state health systems to coordinate seamlessly under one umbrella.
Case Example: From Lab to Public Health Response
Imagine a state lab facing an unexpected spike in respiratory infections.
Without a LIS:
- Data is collected manually and delayed
- Reporting backlogs build up
- Epidemiologists lack real-time case data
With Prolis:
- Samples are barcoded and tracked instantly
- Results auto-route to public health authorities
- Dashboards visualize spread and positivity trends
- Leadership makes timely decisions to contain outbreaks
Speed translates into containment. And containment saves lives.
Why Prolis Stands Out for Public Health Labs
Prolis LIS is engineered to meet the needs of large-scale, distributed laboratory networks.
✅ Multi-site connectivity — centralizes data across public health regions
✅ HL7/FHIR interoperability — enables communication with CDC/state systems
✅ QC and audit logs — maintain data integrity and compliance
✅ Automation-first architecture — scales during surges without downtime
✅ Custom dashboards — visualize outbreak data in real time
For public health agencies, Prolis becomes more than a LIS it’s a data intelligence platform that supports rapid, coordinated response.
The Future: AI-Enhanced Outbreak Management
The next generation of LIS systems will leverage AI to predict outbreak patterns before they escalate.
- Machine learning algorithms can identify abnormal result clusters
- Predictive dashboards can model spread trajectories
- Automated alerts can notify agencies when thresholds are exceeded
Prolis is already developing AI-driven modules to enhance predictive analytics and resource planning empowering public health labs to move from reaction to prevention.
Conclusion: Connecting Data, Speed, and Safety
Outbreak response isn’t just about testing capacity it’s about data clarity.
Public health labs equipped with modern LIS platforms can scale faster, communicate clearer, and act sooner transforming how we detect, respond, and contain public health threats.
With Prolis, public health labs gain the technology infrastructure to lead confidently in crisis from the first specimen to the final report.