RCM Automation in Labs: Your Key to Faster Payments
The Financial Pulse of Every Laboratory
Every laboratory runs on two cycles the testing cycle and the payment cycle. While the former drives diagnostics and patient outcomes, the latter determines sustainability and growth.
Yet, despite the sophistication of modern analyzers and LIS technology, many labs still handle Revenue Cycle Management (RCM) manually leading to delays, denials, and lost revenue.
In 2025, automation isn’t just an operational upgrade; it’s a financial strategy. RCM automation helps labs move from chasing payments to capturing revenue in real time.
This blog explores how automating RCM workflows especially when integrated with your LIS accelerates payments, reduces denials, and builds long-term financial health.
What Is RCM Automation?
Revenue Cycle Management (RCM) automation refers to the use of technology to streamline billing, claim submission, payment posting, and denial management processes.
For laboratories, this means:
- Automating claim creation and submission
- Verifying patient eligibility in real time
- Checking payer rules automatically
- Posting remittances electronically
- Generating performance reports without manual reconciliation
The result: a faster, cleaner, and more predictable payment cycle.
The Problem with Manual Billing Workflows
Manual or semi-automated billing still dominates many labs even those with advanced LIS systems.
Common challenges include:
- Delayed claim submission due to manual data entry
- High denial rates from missing or mismatched information
- Slow AR follow-up due to lack of visibility
- Inconsistent reporting for management and forecasting
Every one of these issues translates directly into cash flow leakage.
In fact, industry studies show that labs lose up to 5–10% of annual revenue due to billing inefficiencies alone.
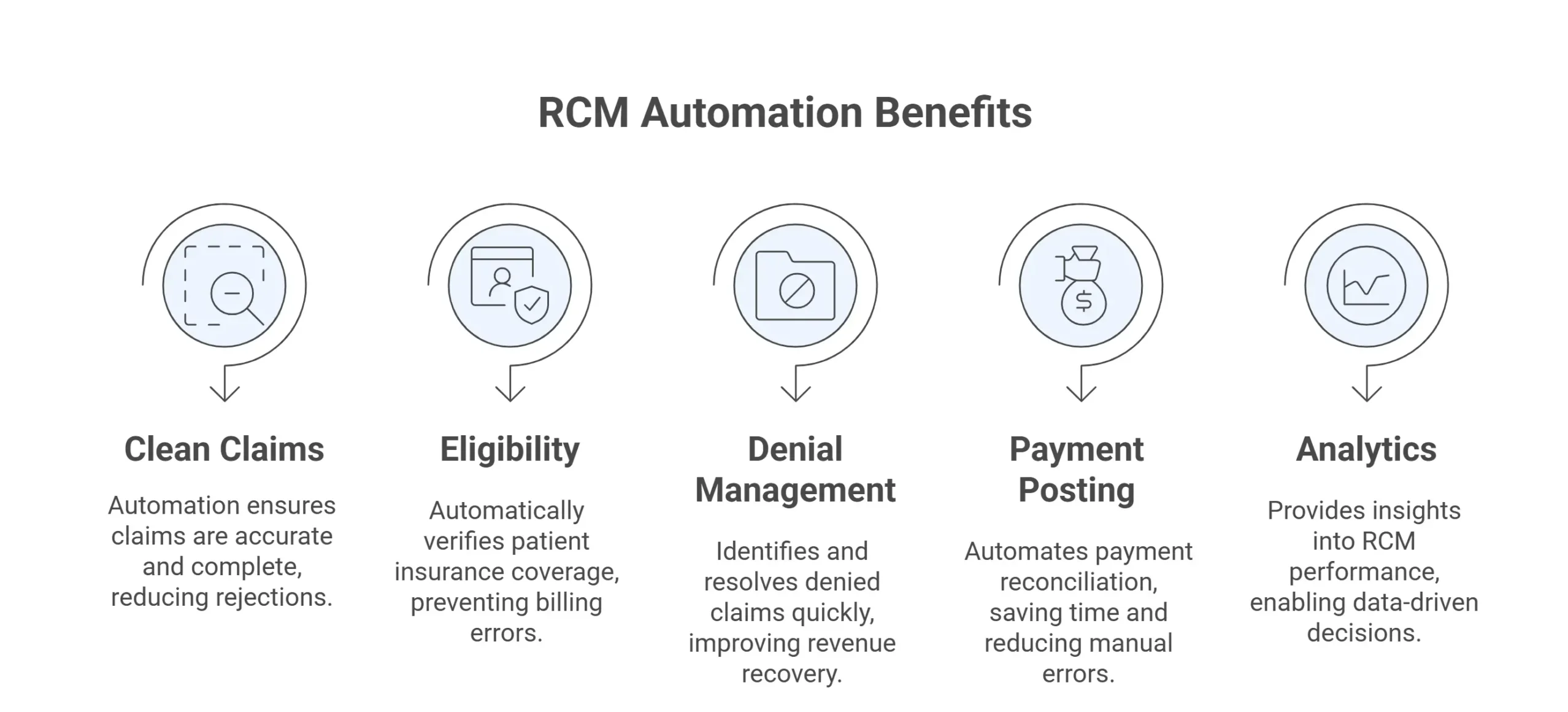
5 Ways RCM Automation Accelerates Payments
Let’s break down how automation transforms the financial health of your lab.
1. Clean Claims from the Start
The majority of denials stem from avoidable errors missing codes, invalid patient data, or mismatched payer details.
RCM automation integrates directly with your LIS to:
-
- Pull verified patient and test data automatically
- Apply payer-specific rules before submission
- Validate CPT/ICD-10 combinations for medical necessity
Result: More clean claims, fewer rejections, and faster payments.
2. Real-Time Eligibility Verification
Manual eligibility checks are slow and often skipped, leading to denials later.
Automated RCM systems run real-time eligibility checks before testing or billing, confirming:
-
- Coverage status
- Policy details
- Co-pay or deductible information
This prevents unpaid claims and improves patient communication before testing begins.
3. Automated Denial Management and Resubmission
In a manual environment, denied claims can linger for weeks.
Automation allows labs to:
-
- Auto-route denials for correction
- Flag repeat issues by payer or test type
- Resubmit corrected claims automatically
By analyzing denial trends, labs can pinpoint recurring root causes turning every denial into a learning opportunity.
4. Integrated Payment Posting and Reconciliation
Automated payment posting eliminates tedious manual entry of remittance data.
With integration between LIS and RCM:
-
- Payments are matched automatically to claims
- Partial or underpaid claims are flagged
- Real-time revenue dashboards show AR performance
This visibility helps labs manage collections more proactively.
5. Performance Analytics and Forecasting
RCM automation isn’t just about transactions it’s about intelligence.
Automated reporting tools provide:
-
- Daily cash flow summaries
- Denial rate tracking
- Aging reports by payer
- Revenue forecasts by test or client
With data-driven visibility, labs can make faster, more informed financial decisions.
Why RCM Automation Matters Now More Than Ever
Payers are tightening rules. Reimbursement rates are shrinking. Compliance expectations are rising.
Automation gives labs the agility to adapt and to scale without adding billing staff.
Labs that have adopted RCM automation report:
- 30–50% faster payment turnaround
- 25–35% reduction in denials
- 10–15% improvement in clean claim rate
- Improved audit readiness and compliance
In an industry where margins are narrow, those gains translate directly into profitability.
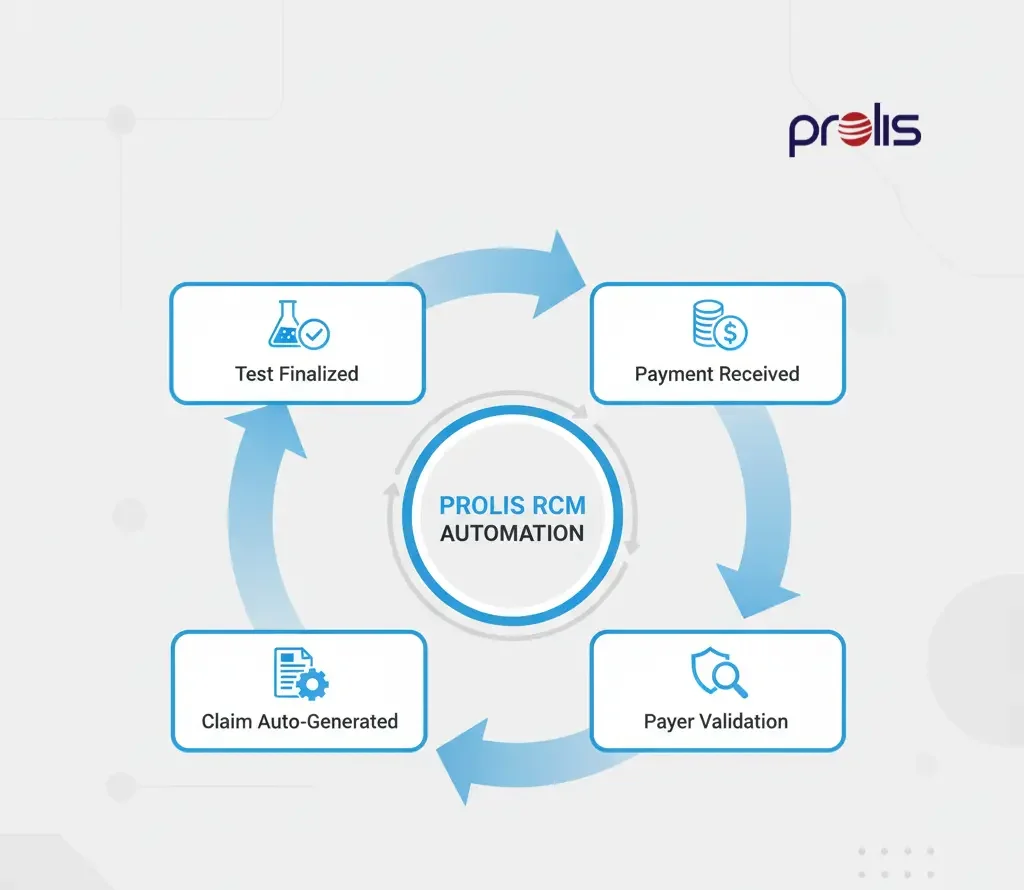
How Prolis Connects RCM and LIS for End-to-End Automation
Prolis integrates billing directly into the LIS workflow eliminating silos and handoffs that cause financial leaks.
Key Features Include:
✅ Auto-claim generation on result finalization
✅ Built-in payer rules engine for pre-validation
✅ AR dashboard for payment tracking
✅ Denial trend analytics
✅ Audit-ready logs for compliance
Prolis bridges the gap between lab operations and billing ensuring that every test performed becomes a test paid for.
The Long-Term Impact: More Revenue, Less Risk
By automating RCM, labs gain:
- Predictable cash flow
- Stronger payer relationships
- Lower administrative costs
- Greater visibility into profitability
Instead of reacting to denials and delays, labs operate proactively improving both operational and financial performance.
RCM automation isn’t just about faster payments. It’s about building a financially resilient lab that can scale sustainably.
Conclusion: Your Lab’s Financial Automation Engine
Every lab has automation in testing. Now it’s time to bring that same precision to billing.
When integrated with your LIS, RCM automation removes the friction between diagnostics and dollars turning billing into a seamless, self-managing process.
With Prolis RCM Integration, labs gain more than speed. They gain control over their revenue, compliance, and financial future.
In a world of shrinking margins, automation isn’t optional. It’s essential.