How Interoperable LIS Systems Improve Lab-Physician Collaboration
From Information Silos to Seamless Collaboration
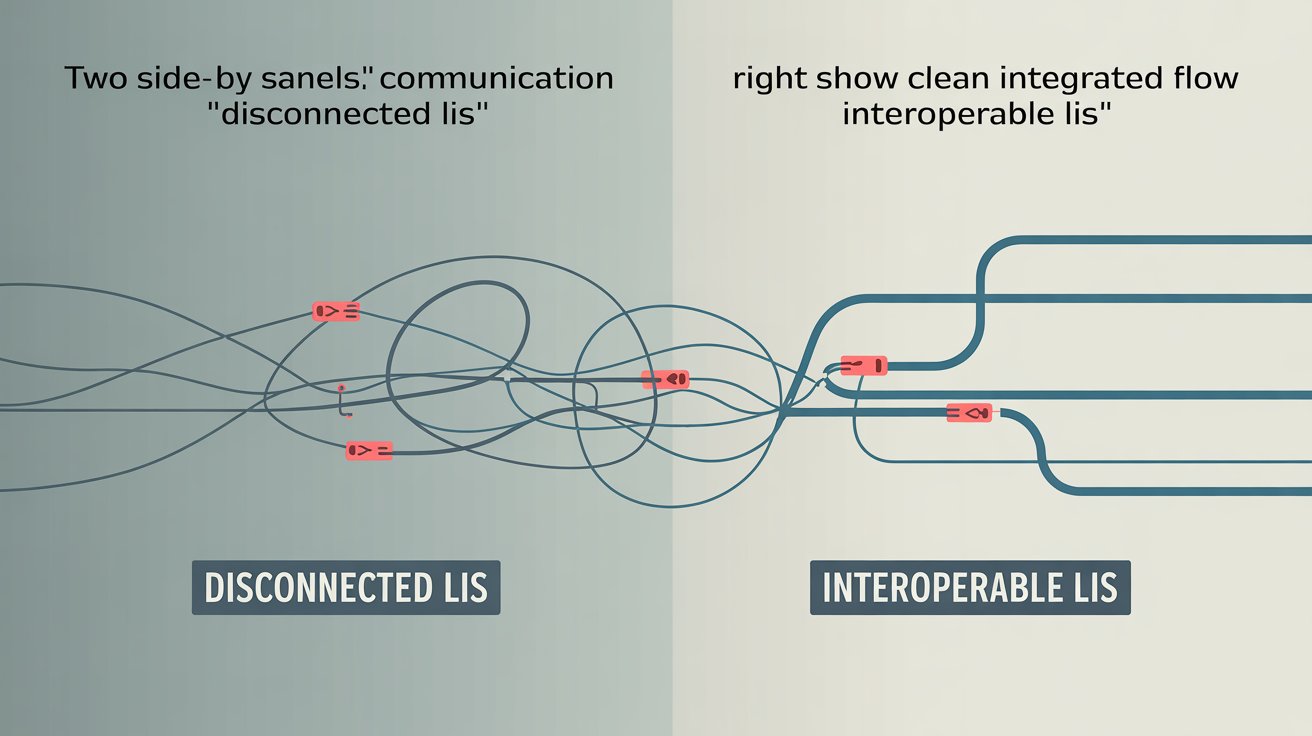
In healthcare, laboratory data drives clinical decisions. But despite this critical role, many labs still struggle to effectively communicate with physicians. Result delivery is delayed, follow-up questions require phone calls, and disconnected systems cause rework.
The core problem? Lack of interoperability. When a lab’s LIS (Laboratory Information System) can’t seamlessly communicate with physician EMRs, portals, and communication tools, the result is a broken feedback loop.
Interoperable LIS systems solve this. They bridge the gap between lab operations and clinical care by enabling real-time, structured, and secure data exchange. The result: faster diagnoses, stronger collaboration, and better outcomes.
What Is LIS Interoperability?
Interoperability means that different software systems like a lab’s LIS and a clinic’s EHR can exchange and interpret data accurately and reliably.
This requires more than just sending PDFs or faxes. Interoperability includes:
- Standardized data formats (e.g., HL7, FHIR)
- Secure, bi-directional connections between systems
- Context-aware data mapping (matching test codes, patient identifiers, etc.)
- Real-time syncing of orders, results, and follow-up communications
Interoperable LIS systems don’t just send data they make collaboration part of the workflow.
The Collaboration Gap: Where Traditional LIS Systems Fall Short
Most non-interoperable LIS setups rely on outdated or manual processes to communicate with physicians:
- Static result reports emailed or faxed
- Providers needing to log into separate lab portals
- No integrated alerts for abnormal results
- Manual follow-up calls for clarification
This slows down care, increases staff burden, and leads to fragmented clinical decisions.
An interoperable LIS eliminates these barriers by embedding communication directly into the ordering, testing, and reporting processes.
5 Ways Interoperable LIS Improves Lab-Physician Collaboration
1. Faster Result Delivery with Fewer Errors
When LIS and EMR systems are connected, results are delivered instantly and directly into the provider’s workflow no logging into external portals or waiting on faxes.
This:
- Reduces turnaround time
- Eliminates manual data re-entry
- Ensures critical results are seen faster
Interoperable LIS systems also support structured data delivery, which allows for automated flagging of abnormal values, reducing oversight risk.
2. Improved Test Ordering Accuracy
Bi-directional interoperability allows physicians to place lab orders directly from their EHR, with those orders flowing immediately into the LIS.
Benefits include:
- Reduced transcription errors
- Complete patient and insurance data included automatically
- Fewer calls back and forth between labs and clinics
An interoperable LIS streamlines pre-analytical steps, reducing confusion and rework.
3. Better Follow-Up Communication
Interoperable LIS platforms support clinical messaging, allowing labs to send comments, follow-up questions, or interpretation notes directly to the provider.
Examples include:
- Suggesting a reflex test based on initial results
- Notifying providers when a sample was compromised
- Delivering interpretive commentary with toxicology panels
This reduces reliance on separate phone calls or emails, keeping all communication inside the clinical record.
4. Integrated Reporting and Clinical Context
Rather than delivering standalone result files, interoperable LIS systems embed reports directly into the physician’s patient record.
This allows:
- Side-by-side viewing of results with vitals, history, and prescriptions
- Better clinical decision-making
- Greater accountability in documentation
When lab data is part of the broader record, providers can act faster and with more context.
5. Reduced Administrative Burden
Labs and clinics spend significant time on follow-up: clarifying orders, tracking down results, resending reports.
Interoperability reduces this burden by:
- Syncing data in real time
- Allowing providers to self-serve results
- Automating routine follow-up steps (e.g., confirmations, flags, report routing)
This frees lab staff to focus on value-added tasks, while providers get answers faster.
Why Interoperability Matters More Than Ever
In 2025, care teams are distributed. Patients expect speed. Regulations demand traceability. And value-based care models reward coordination.
LIS systems that cannot integrate will become liabilities. Labs that adopt interoperable LIS platforms are positioned to:
- Attract and retain high-value provider clients
- Reduce communication breakdowns
- Deliver faster results with less friction
- Meet emerging interoperability standards (e.g., TEFCA, FHIR APIs)
How Prolis Enables True Interoperability
Prolis is designed for end-to-end connectivity with providers, EMRs, billing systems, and external tools.
Key features include:
- HL7, ASTM, and FHIR integration options
- Real-time order and result exchange
- Structured messaging for clinical collaboration
- Configurable report delivery (EHR, secure email, portals)
- Bidirectional data sync for LIS-EMR workflows
Whether you’re working with a solo physician office or a large multispecialty group, Prolis ensures labs become part of the provider’s workflow not a disconnected endpoint.
Future of Collaborative Diagnostics
As healthcare becomes more data-driven, the lab-provider relationship must evolve. Collaboration depends on visibility, speed, and trust all of which are enabled by interoperable LIS systems.
Labs that operate in silos will be left behind. Those that integrate into provider workflows will become essential partners in care delivery.
An interoperable LIS is not just a technical upgrade. It is a strategic investment in better diagnostics, better communication, and better outcomes.